TELEHEALTH
The group facilitating the discussion this week provided the following definition of telehealth: information and computer technology used to support healthcare, services, and expertise over any geographical distance. The group discussed how one of the most important factors in using telehealth technology is that it allows nurses and other health care providers to give care over large geographical distances; therefore, it allows people in remote or rural areas to receive care at home without having to travel large distances.
What is telenursing? What is the role nurses in telenursing?
According to Lorentz (2008) telenursing incorporates all forms of nursing care delivered at a distance through the use of electronic technology. Telecare nursing, a subset of telenursing, is when nurses receive and interpret information obtained from patients through the phone (Lorentz, 2008). Telecare nurses direct and coordinate care to patients, rather than providing hands on nursing care (Lorentz, 2008). Telehomecare nurses are another subset of telenurses; their role is to deliver healthcare services electronically to patients in their own homes. In this mode of care patients are given the necessary home monitoring equipment, and nurses teach the patients and their family how to use the equipment (Lorentz, 2008). Telenurses are responsible to uphold the same standards or practice as other nurses (Schlachta-Fairchild, Elfrink, & Deickman, 2008). However, of College of Nurses of Nova Scotia is the only province in Canada to create nursing guidelines specific to Telehealth.
HUGO
The class discussion explored the HUGO program , and the benefits and challenges that it presents to the health care system. HUGO stands for healthcare undergoing optimization (Walker, 2013) It incorporates the following four components:
(1) a computerized provider order entry (CPOE)
(2) an electronic medication administration record (eMAR)
(3)closed looped medication administration (CLMA)
(4) and electronic medication reconciliation (e Med Rec)
According to Walker (2013) HUGO will benefit the health care system by improving access to health care services, decreasing medication errors, improving patient outcomes, improving medication compliance, improving communication between health care proving, and improving antibiotic therapy. Overall, implementing the HUGO system will streamline services making them more efficient.
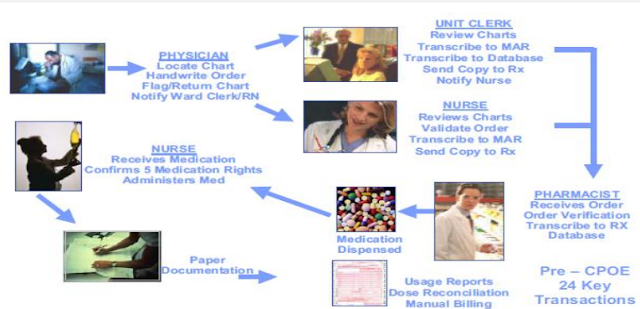
The following images show how HUGO will streamline medication services:
 |
| The medication process with HUGO |
ONTARIO TELEMEDICINE NETWORK
Through researching about telehealth in Ontario, I discovered another ehealth technolgoy used in Ontario to provide care to patients: Ontario Telemedicine Network (OTN). OTN is an independent, not for profit organization funded by the government of Ontario. OTN definies telemedicine as "the provision of health care by means of telecommunications and information technology" (Williams, 2013). OTN provides a variety of services including teledermatology, telestroke, teletrauma, teleburn, telehomecare, teleophthalmology, and mental health services. From 2012 to 2013 in Ontario more than three hundred thousand patient received care through OTN. In addition, the use of telemedicine saved the health care system sixty million dollars in what would have been allocated to patients having to travel to receive health-care as part of the Nothern Health Travel Grant.
In their 2012-2013 report OTN discusses their new telemedicine nurse initiative. The organization is working with the Local Health Integration Networks (LHINs) in Ontario to hire and train 191 telemedicine nurses whose role is to provide virtual patient consultations, conduct assessments, train patients and provide knowledge. OTN has also created a Clinical TMC Certification Program as the best practice standard for nurses working in Telemedicine.
This Video explores how one LHIN in the Ottawa region is using Telemedicine by arranging videoconferencing between physicians and patients to provide care. Research indicates that videoconferencing allows physicians to prescribe treatments immediately which results in less anxiety for patients and prevents further health complications (Lorentz, 2008). After watching the video, the aspect that left the biggest impression with me is how videoconferencing supports a client centered approach to care and how it addresses the social determinants of health.
This video is also from the Ontario Telemedicine Network explores how telehomecare works and how it is benefiting patients. It also explores the role of the telemedicine nurse specialist in providing telehomecare services.
 |
| This image shows the teledermatology service |
How does the use of telemedicine impact the outcomes of patients? How does it impact nursing care?
Scholarly research concerning telenursing explores both the benefits and the challenges it poses to providing health care services. According to Lorentz (2008) the main argument to support telenursing is that is it makes health care services easier to access for patients. Telenursing also supports a client centered approach to health care services, because it eliminates patient's travelling costs in order to access health care services (Lorentz, 2005). Research indicates that telenursing may be especially useful for providing care to people with mobility problems and the elderly. Furthermore research supports that elderly people value telehomecare services; in one study over half of the elderly participants reported that they preferred telehomecare visits using videoconfrencing over face to face care (Lorentz, 2008). In addition, nurses have reported that telenursing is in opportunity to provide more efficient care compared to face to face nursing; in one study nurses reported that 40% of their in home visits did not require hands on care and could be replaced with telenursing (Lorentz, 2008). Another benefit of telenursing is that it allows for more frequent visits to patients and therefore better patient outomes (Lorentz, 2008). For example, in one study the patients of nurses who provided care through telenursing had improved healing rates compared to patients who received face to face nursing care (Lorentz, 2008). In addition to supporting a client centered care approach, allowing patients to save money, and enabling nurses to provide more frequent visits, telenursing has also been proven as an effective means of diagnosing disease(Schlachta-Fairchild, Elfrink, & Deickman, 2008).
Research indicates that diagnosis through telemedicine is just as effective as face to face diagnosis. For example, a study found that remote diagnosis using elecrocardiogram results as just as reliable as interpretation done in person (Schlachta-Fairchild, Elfrink, & Deickman, 2008).
However, research indicates that nurses are concerned about how telenursing impacts the therapeutic nurse-client relationship, including the inability of nurses to use therapeutic touch to communicate with patients (Lorentz, 2008). Other concerns with the use of telemedicine are issues with maintaining privacy and confidentiality, the possibility of equipment malfunctioning, and inaccurate diagnoses due to patient or caregiver errors(Schlachta-Fairchild, Elfrink, & Deickman, 2008). There are also concerns that some nurses may view technology as a tool to replace nursing care, rather than simply a means in which to provide care (Schlachta-Fairchild, Elfrink, & Deickman, 2008).
References
Brown, E., & Marshall, R. (2013). Embarking on the journey for virtual care. Ontario Telemedicine
Network. Retrieved from http://otn.ca/sites/default/files/otn-annual-report-2012-13.pdf
Lorentz, M. (2008). Telenursing and home healthcare: The many facets of technology. Home Healthcare
Nurse, 26(4), 237-43. doi: 10.1097/01.NHH.0000316702.22633.30
Ontario Telemedicine Network (Producer). (2011). Telehomecare 1 min video [video]. Available
from https://www.youtube.com/watch?v=U_W-AE-91Mw
Ontario Telemedicine Network (Producer). (2013). Telemedicine in the Champlain Region [video].
Available from https://www.youtube.com/watch?v=ta8nj4fV6BY
Ontario Telemedicine Network (Producer). (2011). Telehomecare 1 min video [video]. Available
from https://www.youtube.com/watch?v=U_W-AE-91Mw
Ontario Telemedicine Network (Producer). (2013). Telemedicine in the Champlain Region [video].
Available from https://www.youtube.com/watch?v=ta8nj4fV6BY
Schlachta-Fairchild, L., Elfrink, V., & Deickman A. (2008). Patient Safety and Quality: An Evidence-
Based Handbook for Nurses. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK2687/
Based Handbook for Nurses. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK2687/
Walker, R. (2013,
May1-3). Healthcare Undergoing Optimization. [E-Health Summit]. Retrieved from h
Walker, R. (2013, May1-3). Healthcare Undergoing Optimization. [E-Health Summit]. Retrieved from h